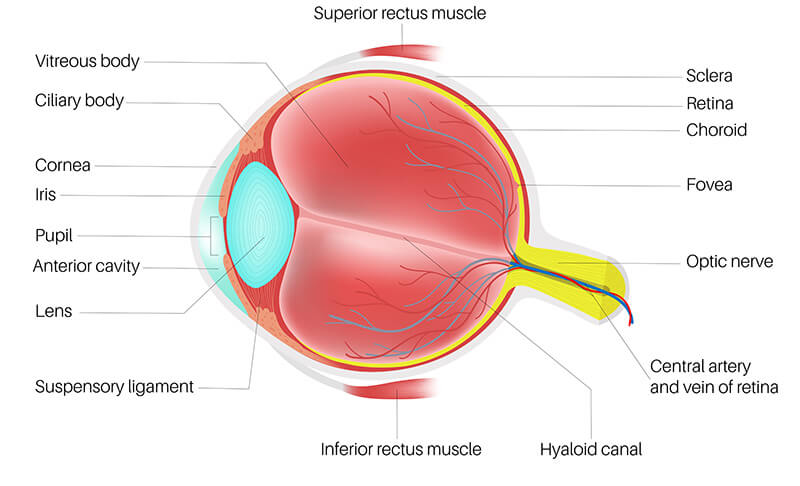
In order to see, light must pass through the cornea, then the anterior chamber, then the pupil (a hole in the Iris), followed by the lens, the vitreous, and finally it is absorbed by the retina. This pathway is called the visual axis. The retina converts light energy into electrical energy that travels down the optic nerve to the visual cortex of the brain.
Since anatomy and pathology are closely related, you’ll find that this section also contains descriptions of the most common causes of visual loss: cataract, glaucoma, and macular degeneration, as well as other common eye diseases like conjunctivitis (pink eye), presbyopia, (arms getting too short), floaters, and retinal detachment.
The cornea is the clear, dome-shaped membrane on the surface of your eye that normally is about 0.5 mm thick (0.002 inches; a dime is about 1.0 mm in thickness). Contact lenses rest on the cornea, and since the cornea has no blood vessels, it receives most of its oxygen from direct contact with the air. So, for the cornea, wearing a contact lens is a bit like trying to breathe through a wet towel. Some types of contact lenses allow more oxygen to pass through than others and are healthier for the eye. The cornea has more pain fibers per unit area than any other place on the body.
The cornea, together with the lens, focus light on the retina, much like the lenses in a camera focus light on the film. About two thirds of the focusing power comes from the cornea. A cross-section of the cornea perpendicular to the visual axis should show a circle, but with astigmatism, a corneal cross-section looks slightly football-shaped. Nearsightedness (myopia) and farsightedness (hyperopia) are also sometimes due to an abnormal shape to the cornea, although they are more often caused by an abnormally large (myopia) or abnormally small (hyperopia) diameter of the entire eyeball. Most current refractive surgeries like Lasik and PRK irreversibly alter the shape of the cornea.
The anterior chamber is simply a space behind the cornea and in front of the iris that contains a clear, nutrient fluid called aqueous humor. The so called “drainage angle” or trabecular meshwork (TM) is also located here. The trabecular meshwork is a circle of specialized tissue where aqueous humor drains out of the eye. It is located at the intersection of the cornea, the sclera (the white part) and the iris (the colored part). When it is damaged, glaucoma is often the result. The majority of patients with glaucoma have the open-angle type; anatomically the angle is open and fluid flows up to the TM, but microscopically the TM is clogged. Unfortunately, fluid inside the eye is continuously produced by the ciliary body, and when the TM is clogged, the pressure in the eye rises above normal. High pressure literally crushes the optic nerve which becomes progressively damaged and vision is slowly lost.
A minority group of people with glaucoma have narrow angle or angle closure glaucoma. In these people, the iris mechanically blocks the trabecular meshwork and their eye pressure can rise suddenly, with abrupt onset of pain and vision loss. Most people with glaucoma have a very slow and completely painless vision loss.
The pupil is literally a hole in the paper-thin iris, the front of which gives the eye its color. The iris is actually one part of a continuous layer which wraps itself around the inside of the eye called the uvea. The parts of the uvea include the iris, the ciliary body (a tire-like structure at the root of the iris) and choroid (a thin pigmented layer located in between the sclera and retina). The iris contains a circular muscle at the edge of the pupil that constricts the pupil in bright light and radial muscles, like spokes on a wheel, that dilate the pupil in low light. Inflammation of the iris is called iritis or uveitis, a painful condition characterized by sensitivity to light.
The lens is shaped just like a round, magnifying lens (think chocolate M&M.) It is located behind the pupil and iris and is attached to the ciliary body by hundreds of thread-like zonules. Optically, the lens works together with the cornea to focus light on the retina. When the lens is cloudy or opaque, it is called a cataract. Cataracts are present, at least to a small degree, in virtually everyone over 60 years of age, but can occur in people of any age, even in newborns. There is a thin capsular membrane surrounding the lens (the “candy layer” of the M&M). During cataract surgery, a circular hole is created in the front or anterior, surface but the back posterior, surface is left intact to support the lens implant, and to prevent the vitreous from herniating forward.
Remarkably, the lens also has the ability to accommodate. Accommodation describes the ability of the lens to change its shape (thicken) in response to contraction of a band of muscle within the ciliary body, thereby changing its power, allowing us to focus on near objects. Between ages 42 and 65, the lens slowly hardens and loses its ability to accommodate. The loss of the ability to accommodate with age is called presbyopia. People with presbyopia need glasses to read. Everyone becomes presbyopic, although myopic people retain their ability to read without glasses as they age.
The vitreous or Vitreous Humor is a semi-solid, fibrous gel. By and large the vitreous is clear, but is also may contain fibrous bands and firm attachments to the retina. There is one area of the vitreous in particular that is thickened and opaque called a Weiss Ring; normally this little attachment rests on the head of the optic nerve. Since the optic nerve head is the natural blind spot in our vision, you can’t see this bit of vitreous. Eventually, however, this little attachment separates from the optic nerve head and you can see it floating about on the inside of your eye. Often it apears to be a circle, a web, or an insect-like configuration. New floaters are usually harmless, but occasionally they signal the beginning of a retinal detachment, intraocular bleeding, inflammation, or infection.
The retina is a thin film of tissue that coats the inside of the eye. If you were to impale a sharp object into the white part of your eye, it would first pass through the conjunctiva, a clear protective layer that turns red if you rub your eye (infections of the conjunctiva are called conjunctivitis, or pink eye), then sclera, the tough, protective white part of the eye, then choroid, a pigmented layer and component of the uveal track, then retina, the nervous tissue that converts light to an electrical signal, then finally the vitreous cavity. The retina is highly organized, with 10 layers of cells, and has blood vessels running through it that provide nutrients, like oxygen, but these superficial vessels only bring in enough nutrients for the inner two-thirds of retinal cells. The outer third of the retina gets its oxygen and nutrients from blood vessels in the choroid. A retinal detachment is said to occur when the retina separates from the choroid. For example, if a break forms in the retina, fluid from the vitreous goes underneath the retina, and the retina peels away from the choroid. Since the outer one third of the retina gets its nutrients from the choroid, these cells quickly die away. The pattern of blood vessels on the surface of the retina varies from person to person, and in fact can be used as a unique personal identifier.
Having a retinal detachment doesn’t necessarily lead to blindness if only a small area of peripheral retina was detached. As you read this print, light rays originating from the words are striking your retina in a highly specialized area called the macula. Still looking at the screen, you can also see, in your peripheral vision, your mouse, and your desk. The macula has the highest acuity (and the best color vision), but it only covers a very narrow range and it only works in relatively bright light. Using your peripheral vision, you can’t read the writing on your mouse, but using your macula, you can. On the other hand, if you are trying to navigate around the house, your peripheral vision is what keeps you from bashing into door frames and furniture. If you only had your maculas, walking in the house would be like trying to map out the inside of a dark room using only a narrow-beamed flashlight. Another feature of the peripheral retina is that it is much more sensitive to light than the macula. In fact, in very dim light, your maculas are hardly working at all. Pilots are trained to use their peripheral vision when flying at night for this reason.
Macular degeneration is, unfortunately, a relatively common disease in the elderly where the maculas (a specialized part of the central retina) degenerate and can no longer function. In the worst cases, central vision is completely lost in both eyes. Imagine holding a grapefruit a few inches in front of your face, and you’ve got a pretty good idea of what can happen visually. Patients with macular degeneration maintain their peripheral vision, so they can continue to function independently, but the lack of central vision makes reading, driving and most other visually demanding activities difficult. Fortunately, the majority of people diagnosed with macular degeneration will maintain reasonable central vision throughout their lives, and some people will have no visual loss whatsoever. Everyone who has been diagnosed with macular degeneration should test their vision daily with an Amsler Grid.
If you think of the eye as a hollow ball, the inside layer is coated with several layers of retinal cells. Very thin, thread-like nerve fibers travel from the retinal cells along the innermost layer of the retina and join together in a bundle called the optic nerve. The head of the nerve is about 1.5 mm in size, and is visible inside the eye, just as it passes through a hole in the sclera on its way to the brain. Anatomically this hole is really more like a window with a screen over it, and there is no retinal tissue here, so this creates our natural blind spot. In the left eye, the blind spot is about 15 degrees to the left of our central vision (fixation), and in the right eye the blind spot is 15 degrees to the right of fixation. When the pressure inside the eye rises (glaucoma), this spot also happens to be the most vulnerable to pressure, so the optic nerve is literally crushed, and it slowly dies. For some reason, the nerve fibers that go to our mid-peripheral vision die first, so glaucoma is characterized by peripheral vision loss in a characteristic pattern. Unfortunately, just as we aren’t aware of our natural blind spot, we also are not aware as new blind spots develop until peripheral vision loss is very extensive. Vision loss from glaucoma is irreversible.
Even though glaucoma is due in large part to abnormalities in the trabecular meshwork that impede the flow of fluid out of the eye, visual loss from glaucoma occurs due to progressive damage to the optic nerve. Glaucoma is in fact the most common disease affecting the optic nerve, and is classified medically as a type of optic neuropathy.