Migraines are notorious for their ability to disrupt daily life, causing debilitating pain, nausea and sensitivity to light and sound. Despite over a billion people living with and suffering from migraines worldwide, the complexity of this neurological disorder is not often at the forefront of discussion when it comes to the seriousness of chronic pain management. The terms headache and migraine are frequently used interchangeably. Sometimes migraines are thought to be a more intense or severe kind of headache. Under the umbrella category for migraines, there is a distinctive subtype known as ocular migraines. The disparities between ocular migraines versus regular migraines have key differences; understanding them is imperative for accurate diagnosis and effective treatment.
Let’s begin with a basic definition of the 2 types of migraines. Regular migraines are denoted by moderate to severe throbbing, pulsating pain usually on one side of the head. Ocular migraines, on the other hand, are uniquely characterized by disturbances in vision that precede or accompany the headache. These visual intrusions, also called auras, are the hallmark of telling the difference between regular and ocular migraines. Auras are usually temporary and can include zigzag lines, flashing lights, blind spots or shimmering lights. Common triggers for regular migraines include stress, hormonal changes, lack of sleep, certain foods and environmental factors such as strong odors or bright lights. While ocular migraines share some stimulating factors with regular migraines, such as stress and hormonal changes, they may also be linked to specific visual prompts, such as intense lights or patterns.
Regular migraines often have a longer duration, ranging from a few hours to up to 72 hours in some cases. Individuals who suffer from regular migraines may experience attacks several times a month. Ocular migraines typically have a shorter time span, with visual disturbances lasting around 5 to 30 minutes. While the headache that follows the aura may last for a few hours, if at all, ocular migraines are generally less frequent than regular migraines.
Migraines are thought to involve a combination of genetic, neurological and environmental factors that lead to abnormal brain activity, including changes in blood flow and neurotransmitter levels. The exact mechanisms causing ocular migraines are not well understood, but they are believed to involve changes in blood flow to the visual areas of the brain. Navigating treatment options for both types of migraines includes identifying the factors that cause the onset of symptoms, making lifestyle modifications, utilizing pain medication and seeking the expert advice of a trusted ophthalmologist.
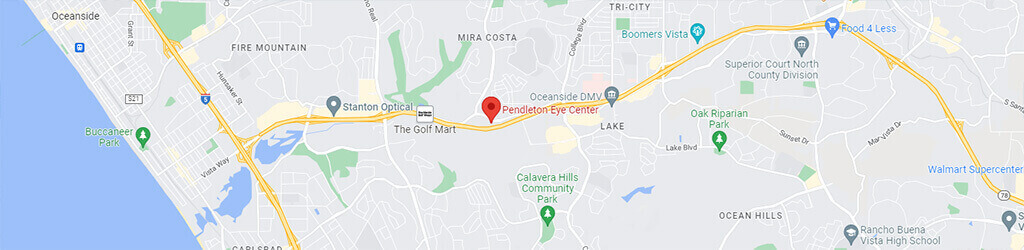
Equipped with a better understanding about ocular migraines versus regular migraines and their key differences, patients can better describe to their doctors the symptoms that accompany significant headache pain and visual disturbances. For vision clarity and pain management, contact Pendleton Eye at 760-758-2008 or WEBSITE.